The NRTO is an international community focused on rare ovarian cancer. It brings together researchers with expertise in the field of rare tumors of the ovary, associated collaborators, patients, patient advocates, clinical ambassadors and patient foundations around the globe.
The project
The mission of The Network of Rare Tumors of the Ovary (NRTO) is to bring together clinicians, scientists, charitable patient advocacy groups, patients and their families to further understanding of rare non-epithelial ovarian tumors. Specific goals include:
The project goals:

Informative portal with links to key information and resources as well as to research registries and biobanks for professionals and affected families.

Promote participation
Helping systematic collection of clinical data and biological samples of patients with rare tumors of the ovary.

Support research
Through the participation in registries and biobanks, patients will support and participate in open-access patient-derived experimental models.
The registries and biobanks:
Their common goal is to collect clinical information and biological samples that support research to improve knowledge of each disease and the genetic variants that predispose to its development. Their shared ultimate goal is to improve outcomes for patients through targeted research. Details of each Registry’s activities can be found on their respective websites, The SCCOHT-SMARCA4 Registry and Biobank and the SCSTs Registry and biobank.
Participating in this cancer research program by registering and donating your tumor and or blood samples is a valuable way to contribute to scientific progress, personalized medicine, and the fight against cancer, while potentially benefiting from access to innovative treatments and contributing to improved outcomes for future patients.
The registries and biobanks:
Their common goal is to collect clinical information and biological samples that support research to improve knowledge of each disease and the genetic variants that predispose to its development. Their shared ultimate goal is to improve outcomes for patients through targeted research. Details of each Registry’s activities can be found on their respective websites.
Participating in this cancer research program, registering, and donating your tumor and or blood samples is a valuable way to contribute to scientific progress, personalized medicine, and the fight against cancer, while potentially benefiting from access to innovative treatments and contributing to improved outcomes for future patients.
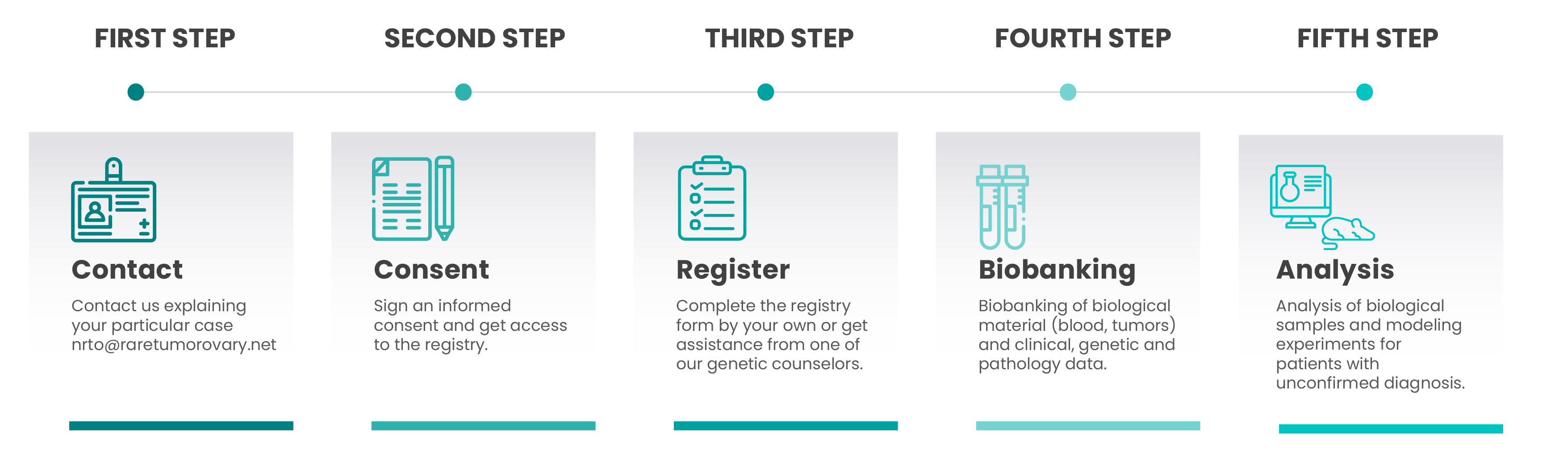
Step1: Contact us explaining your particular case.
Step 2: Know more about SCTCs or SCCOHT registry and biobank.
Step 3: We will reach you and help you through the process consisting of:
signing an informed consent and getting access to the registry.
Step 4: Once you have access, complete the registry form by your own or get
assistance from one of our genetic counselors.
Step 5: We will contact you again to collect and biobank clinical, genetic and
pathology data as well as biological material (blood, tumors) when available. In
parallel, we will perform genomics of the blood and/or tumors with unconfirmed
diagnosis to aid on histological classification and molecular
characterization.
How to navigate this website?
Are you a patient or a carer of SCCOHT or SCSTs?
If your answer is “yes”, you may want to begin by navigating to our homepage, clicking on ‘The Registries’, and selecting the type of tumor that is of concern to you. You will be redirected to other pages and sections. As there is a wealth of information available, it may prove beneficial to take notes and revisit the website multiple times to enhance comprehension.
What content can you find?
You can access information that assists in understanding your diagnosis and navigating this illness, as well as grasping the importance of being connected with this network. On the homepage, you can delve deeper into the project behind this website and contribute to the Patients Registries and biobank. We recommend sharing this website’s information with your medical team. Should you have any doubts, missing information or require clarification, feel free to contact us. There are numerous resources available, so be sure to visit and revisit the website regularly, at your own pace, trying to find answers to your questions, but also exploring its contents to perhaps uncover things you didn’t anticipate.
How can you use the information gathered on this website?
- Share with your doctor to discuss medical options (including open clinical trials);
- Collaborate on patient registries;
- Donate to biobank
- Share with other patients and carers
What are patient-derived experimental models?
Patient-derived experimental models are created by using a small piece of the patient tumor and inserting it under the skin or in an organ in a mouse (patient-derived xenograft) or growing the cells from the tumor in a dish (patient-derived cell model). We can also grow blood cells from the same patient in dish to represent normal cells. In all cases, growing the cells in a laboratory setting mimics how the cells from the patient behave when growing in the human body.
How experimental models can help to cancer patients and caregivers?
Once tumor cells are growing in the lab, we can:
–Study how the disease develops: scientists look at genes and proteins in the growing tumor cells and compare what they see to the normal cells from the blood to find what is unique to the tumor. This is sometimes referred to as identifying tumor “drivers”.
–Test new potential therapies: Researchers can add new potential chemotherapies (chemical compounds) to the growing cells in a dish to identify which compounds can kill the tumor cells, but not kill the normal cells. Then, they can treat mice that bear growing tumor xenografts with these new potential treatments, or use new combinations of known drugs, to see if they are effective at shrinking the tumor growing in the mouse, in the same way they would treat a human patient. This step is unfortunately necessary because not all drugs that can kill tumor cells in a dish are effective at killing the cells of a tumor growing in a living organism. They also need to evaluate the dosage needed because some drugs can have toxic effects on the living organism at the dose required, which scientists need to identify before using the drug on human patients.
–Study drug resistance: Sometimes tumor cells start growing again after treatment (recurrence) or stop responding to treatment during therapy. Here researchers will look again at genes and proteins to see what changed in the growing tumor cells that continue to grow after being exposed to the treatment. They will use that information to modify the treatment strategy and overcome treatment resistance (e.g. test different doses of drugs, or different combinations used together).
Usually, the next step after research using model systems is to run human clinical trials to test the effectiveness of the new proposed treatment. But when dealing with a rare cancer, there are not enough patients to run conventional trials that require statistical analyses and a placebo group. So, the next best option is to use the information gained from one patient’s tumor in “mouse trials” to guide better treatment for the next patient with a similar disease, which is why it is so important for every patient who can participates in research to do so.
If you have any questions, please contact us!
nrto@raretumorovary.net